Case study: Mother wants sickle cell research to change Londoners’ lives
Read Dr Ore-Ofe Ajeigbe's research story.
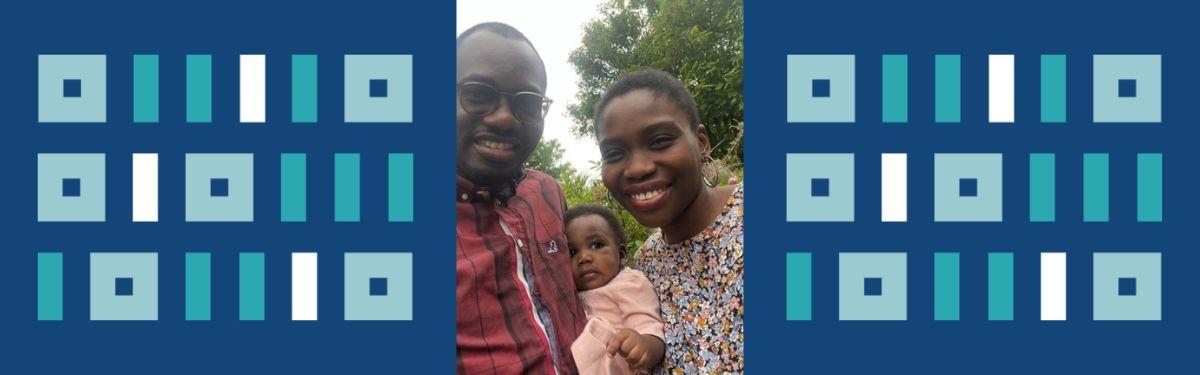
A devoted mother with sickle cell disease wants to build a better world for others with the condition by supporting south London research.
Sickle cell disease is a group of inherited genetic conditions that affect red blood cells. People with sickle cell disease produce unusually shaped red blood cells that can cause problems because they do not live as long as healthy blood cells and can block blood vessels.
Dr Ore-Ofe Ajeigbe, 34, who lives in Kent, took part in the TAPS2 feasibility trial at Guy’s and St Thomas’ NHS Foundation Trust from July 2022 to October 2022. The study aimed to establish how effective a treatment called Serial Prophylactic Exchange Blood Transfusion (SPEBT) is for improving women’s and babies’ health in pregnant women with sickle cell disease.
In SPEBT, sickle blood is mechanically removed and simultaneously replaced with donor red blood cells. The NIHR Clinical Research Network (CRN) South London supported the TAPS2 study by recruiting volunteers.
Ore-Ofe said: “When I am in a sickle cell crisis, the pain can be so bad that I don’t know whether or not I will die. You are desperate for the pain to stop. I feel bad whenever I’m in a crisis as I want to be there for my baby, IseOluware. I don’t want her earliest memories of me to be seeing me in the hospital. Thankfully, there is no chance my daughter will have sickle cell disease as my husband isn’t a carrier.
“I was terrified about managing my first pregnancy with sickle cell disease, but this trial took away those fears. The treatment was genuinely life-changing because it took away my pain. I could enjoy my life, my pregnancy and plan for the future. I cannot thank the Guy’s and St Thomas’ team enough. They looked after me, and the consultant leading this trial went above and beyond for me.
“I would be very happy to take part in research again. Science and medicine have come a long way in the last 50 years. One of the reasons it has come such a long way is because of people taking part in research to help clinicians make things better for future generations. We all have a part to play, and I urge others to volunteer in sickle cell disease research to help their children, grandchildren and future generations.”
Ore-Ofe had regular blood tests before having her blood transfusions as part of her involvement in the TAPS2 feasibility trial. The mother’s final blood transfusion was in October 2022. She gave birth to her daughter in November 2022.
Sickle cell disease is common in people from a black African or Caribbean background. In England, the condition affects around 15,000 people. According to the National Institute for Health and Care Excellence, the condition is also on the rise in people with a mixed ethnic background.
It is a serious and lifelong condition which can cause regular hospitalisation, although treatment can help manage many symptoms. The disorder is also prevalent in the Eastern Mediterranean, the Middle East, India, the Caribbean, and South and Central America.
You can find out about the latest sickle cell research taking place across the capital on the Be Part of Research website.
Picture caption: (L-R) - Dr Mayokun Ajeigbe, Dr Ore-Ofe Ajeigbe, and their daughter IseOluware Ajeigbe.